This is the first of a three post series on the failure of external accreditation mechanisms to make the US Health Care Industry safer. The first post will serve as background and discuss the current state of Clinical Safety, while the next two will discuss All Hazards Natural Disasters and Biological Agents, while the third in the series will focus on Man-made Hazards such as Active Shooters, Terrorism and Workplace Violence in Health Care and a summary of thoughts on how and why this is such an intractable problem give the billions of dollars spent to improve safety in the industry.
Current State: Accreditation has Failed to Improve Outcomes
The Skinny on TJC Accreditation (BMH, posted on September 9, 2014 by Abby Norman) caught our attention and started us thinking about all the Nation’s healthcare external evaluation mechanisms. Since The Joint Commission has enjoyed a near monopoly in the industry we will use its mission statement as a starting point, and continue with some observations about how this mission has not been achieved.
 The stated mission of TJC: “To continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and valueâ€.
The stated mission of TJC: “To continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and valueâ€.
We felt it would a good opportunity to respond with what in our opinion should be a more critical view  of entire external accreditation system, most of the oversight deeming entities – TJC, HFAP and DNV - and TJC in particular. Founded in 1951, JCAHO (now TJC) has enjoyed a close relationship with Congress and the Veterans Administration (VA) and quickly became a quasi-monopoly, receiving an enormous amount of goodwill from those responsible for oversight of the organization. TJC has grown to be the premier global accrediting authority in the US,  boasting 20,500 clients and through Joint Commission International (JCI), they have expanded to many other countries, offering accreditation often required to qualify for US contracts (Military, VA, State Department, Selected Corporate) abroad.
As with all large and bureaucratic organizations, especially those in a position to virtually monopolize the market without determined oversight, TJC has developed some conflicts of interest in the market and in some cases become a victim of regulatory capture by some of the largest organizations in the industry. This was most clear when after finally incorporating strong Emergency Management standards into the accreditation program, TJC climbed down and did not score the new standards after the industry balked. As early as 1998, TJC, then JCAHO, had come under criticism by its’ own regulators, as stated in the Presidential Advisory Commission on Consumer Protection in March 1998:
“Conflicts of interest can arise from multiple sources. For example, private sector accrediting bodies have, as one of their customers, the entities that the organization accredits. The organizations to be accredited sometimes are the organizations that fostered creation of the accrediting entity, and often are necessarily involved in identifying the standards to which they will be accountable.â€
We will break out the clinical and safety/security categories below, but from an overall perspective of Quality, Access and Affordability, a recent Commonwealth Fund report suggests that the US Healthcare System continues to lag other advanced economies, despite a whopping 18% of GDP being thrown at the problem. While we do not agree with several issues raised in the report, an objective claim can be made that the US spends too much for too little and does not provide enough access to care. This interactive chart (tool) we developed makes some global country comparisons and shows how the US has slipped in terms of spending and longevity versus other advanced economies.
We view accreditation as the key mechanism that should offer a steady rate of improvement in measurable quality and results in both Clinical and Physical Safety and Security. Unfortunately, the facts speak for themselves in both of these areas; we have not seen the benefits of continuous improvement, and in our opinion, the quasi-monopoly accreditation structure and lack of competition in setting and measuring the performance standards has hindered, rather than advanced the healthcare industry’s ability to continuously improve. We have long said in posts and our books that TJC accreditation is necessary, but not sufficient to keep patients safe, especially in our specialty discipline of physical safety and security and emergency management.
Clinical Care: Diagnosis, Treatment and Outcomes
Primum non nocere (First, Do No Harm) There are two essential categories of  Safety and Security. The first is Clinical and is focused on the quality of care, prevention of medical errors, and keeping the patient safe during their hospital stay from a medical treatment perspective. In this area, we are not experts, but can cite several examples from those who are:
 “To Err is Human“, the seminal work published by the Institute of Medicine (IOM) in 1999, opened the industry’s eyes to the fact that as many as 98,000 patients died as a direct result of medical error in the diagnostic, therapeutic, preventative and other categories of care. There was the predicable hue and cry in the industry as medical error was shown to be a leading cause of preventable death in the country. But, as with many pronouncements, the urgency died down and the industry settled back into a routine within a few years.
“To Err is Human“, the seminal work published by the Institute of Medicine (IOM) in 1999, opened the industry’s eyes to the fact that as many as 98,000 patients died as a direct result of medical error in the diagnostic, therapeutic, preventative and other categories of care. There was the predicable hue and cry in the industry as medical error was shown to be a leading cause of preventable death in the country. But, as with many pronouncements, the urgency died down and the industry settled back into a routine within a few years.
To Err is Human – To Delay is Deadly - Ten years later, a million lives lost, billions of dollars wasted, published by the Consumer’s Union in 2009, was a follow up to the initial study, which found that little progress had been made, and estimated using CDC numbers, that in the area of Hospital Acquired Infections (HAI) alone, there were about 100,000 deaths a year in the US. According to the report:
“Despite this initial flurry of activity (after the To Err is Human report) , progress slowed once the media moved on to the next crisis. When the IOM published a follow-up report in March 2001, the release barely registered. By 2004, the deadline for the IOM’s goal of a 50% reduction in errors, no national medical error reporting bills had been passed and the initial outrage surrounding the report had faded. Movement towards systematic change to the health-care system remained “frustratingly slow.â€
A September 2013 new, “Evidence-based Estimate of Patient Harms Associated with Hospital Careâ€Â paper from the Journal of Patient Safety reports that deaths from preventable medical errors are in the range from 210,000 to 400,000 per year:
“Using a weighted average of the 4 studies, a lower limit of 210,000 deaths per year was associated with preventable harm in hospitals. Given limitations in the search capability of the Global Trigger Tool and the incompleteness of medical records on which the Tool depends, the true number of premature deaths associated with preventable harm to patients was estimated at more than 400,000 per year. Serious harm seems to be 10- to 20-fold more common than lethal harm.” (emphasis added).
This means millions of incidents of serious harm to patients, an outrageous number, in an environment that was not outrage-fatigued, as America seems to be in the light of no legislative action (or even deep discussion) in this area.  As opined in Forbes:
“If you aren’t alarmed enough that our country is burying a population the size of Oakland every year, try this: you are paying for it. Hospitals shift the extra cost of errors onto the patient, the taxpayer and/or the business that buys health benefits for the infected patient. My nonprofit, which provides a calculator of the hidden surcharge Americans pay for hospital errors, finds most companies are paying millions or even billions of extra dollars for the cost of harming their employees.”
And follows with this:
“The reason many hospital leaders fail to put a priority on safety is that we as a country haven’t forced them to do so. On the contrary, we haplessly pay them for these errors. We tolerate hospital lobbyists insisting on hiding their error rates. We fail to insist on safety when we choose where to seek care or when we put together our business’ health benefits. When we don’t demand safety, they don’t supply it.
It’s time for Americans to make clear to hospitals that they must earn our business, and our trust, and we will not pay with our lives for their failure to act.â€
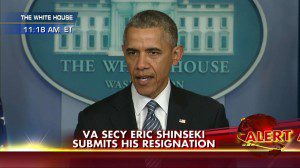 Finally on the clinical side, the recent Veterans Administration healthcare scandal can serve as an excellent case study in the effectiveness of accreditation and TJC accreditation. TJC has enjoyed a monopoly with the VA for decades; just in the past ten years that means there would have been literally thousands of surveys of the 500+ VA hospitals and clinics. Despite this and many other warnings from the OIG and input from the Presidential transition team, TJC singled out the medical center in Phoenix, the one at the center of the 2014 scandal, as one of the top 20 hospitals in the nation in its 2010 report to Congress.
Finally on the clinical side, the recent Veterans Administration healthcare scandal can serve as an excellent case study in the effectiveness of accreditation and TJC accreditation. TJC has enjoyed a monopoly with the VA for decades; just in the past ten years that means there would have been literally thousands of surveys of the 500+ VA hospitals and clinics. Despite this and many other warnings from the OIG and input from the Presidential transition team, TJC singled out the medical center in Phoenix, the one at the center of the 2014 scandal, as one of the top 20 hospitals in the nation in its 2010 report to Congress.
Our next post in this series will examine the other Side of Safety and Security; Physical Safety and Security and All Hazards Preparedness.





0 Comments