Mirror, Mirror on the Wall, 2014 Update: How the U.S. Health Care System Compares Internationally
Executive Summary from Mirror, Mirror
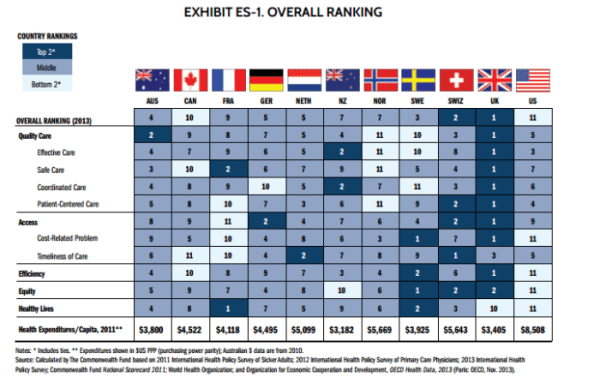
“The United States health care system is the most expensive in the world, but this report and prior editions consistently show the U.S. underperforms relative to other countries on most dimensions of performance. Among the 11 nations studied in this report—Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States—the U.S. ranks last, as it did in the 2010, 2007, 2006, and 2004 editions of Mirror, Mirror. Most troubling, the U.S. fails to achieve better health outcomes than the other countries, and as shown in the earlier editions, the U.S. is last or near last on dimensions of access, efficiency, and equity. In this edition of Mirror, Mirror, the United Kingdom ranks first, followed closely by Switzerland (Exhibit ES-1).â€
The first paragraph pretty much sums it up: According to the latest Commonwealth Fund survey, the US healthcare system apparently underperforms other advanced economies across the board in terms of Access, Efficiency and Equity. That the US spends significantly more per capita on healthcare with shorter lifespans has been demonstrated by World Bank research and CHCER has analyzed similar World Bank data, which shows that while America has been an outlier for many years, some countries (Luxembourg, Switzerland, Norway) have trended toward US levels, rapidly accelerating from 2007. This can be seen by using the year-toggle on this interactive chart.
This is an explosive political issue; the Affordable Care Act has polarized Americans more than any legislation in the last generation. The Commonwealth report will be used (out of context) by pundits and talking heads on both sides to make their relative points, regardless of any “truth†that can be found in the middle of the arguments. And few will honestly look at the true underlying concerns of Access, Quality and Affordability that are the real issues that need to be addressed.
Leaving politics aside and in an effort to understand why the results may be showing such a wide discrepancy, there are several areas to examine more closely in the report, most important being in the areas of survey methodology and resulting data. Some important questions include:
1)Â Â Â Â Comparability
Are the results comparable? The key point is that the US does not offer universal health care insurance, which has a large impact on all the major Quality, Access and Affordability measures, especially for the poor. Fix this and most of the problems will be gone. Got it.
Comparing single payer and multi-payer systems in homogenous and diverse demographic environments is very difficult to do accurately; Japan’s government paid, price-controlled, homogenous cultural system is much different than the UK’s government paid, (with some exceptions),culturally diverse one; and the US has several systems serving very different populations: Medicare, Medicaid, VHA and DoD systems paid by the government, a large chunk of private insurance payers, and fee for service for elective procedures.
2)Â Â Â Â Methodology
Is there bias? Clearly Commonwealth advocates a single payer system. There are some examples that should behave more like single payer systems in the US market – All eligible veterans (6.5M) are covered up to 100% by VHA and all active military and their families (9.5M) are covered 100% by DoD. Recent reports cite many long-standing deficiencies in both of these single payer systems.  In presentation, stack ranking is one way to show differences in survey samples, but frequently it requires subjective calls to be made in the case of ties; is the US getting the short end for tie-breakers? Valid samples and statistically significant results are the standard method of showing results for this type of report.
The survey approach is largely qualitative and based on interviews with patients (demand side), doctors (supply side indirectly self-rating) across multiple years, with OECD statistics sprinkled in to answer some questions. It remains a big mystery how the data is so divergent. For example, 2010 World Bank Per Capita Healthcare Spending is approximately $1,500 in Korea with an average lifespan of 81 years; results for the US are $8,362 and 78 years respectively. Single payer is not the only issue driving this difference. The big question is how to measure effective outcomes in relation to access and affordability, a herculean task that will take years of comprehensive standardized data to accomplish.
3)Â Â Â Â Unconventional Wisdom
UK #3 in timeliness? Depending on how the data is cut across populations, age and income segments, type of illness, etc. the data can show a lot of things. This is one that runs counter to conventional wisdom. Additionally, while the UK gets the overwhelming praise for all areas, the report summary begins:
“The U.K. continues to demonstrate strong performance and ranked first overall, though lagging notably on health outcomes.†Arguably, outcomes are the most important measure of all. This begs the questions:
UK is #1 in Quality of Care, Effective Care, Safe Care, Coordinated Care and Patient-Centered Care – but lags on Outcomes? And,
Why aren’t the Health Outcomes published for every country, and more notably why wouldn’t the methodology add a weighted importance factor for that criterion?
4)Â Â Â Â Measuring Quality in Healthcare
Experts across the globe have been debating the issue of measuring healthcare quality for decades; ISO, EFQM, Baldridge, TJC, DNV, CMS and others have reams of guidance and methodologies on how to measure performance, effectiveness and quality for clinical and administrative areas. Given there are no universally accepted international standards, the Commonwealth methodology to measure quality provides some broad measure of a general direction, but is not nearly precise enough to justify the kind of conclusions that are presented.
5)Â Â Â Â The Role of International Accreditation Mechanisms
Despite all of the above issues and concerns, it is still difficult to determine the real causes and effects on quality of care. Most hospitals in the countries covered would have to be accredited at a national and or local level to operate. The Gold Standard for accreditation has been Joint Commission International (JCI), a subsidiary of The Joint Commission,(TJC).
Incorporating ISQua and other international standards in the late 1990’s, TJC (then JCAHO) introduced the JCI Standards in 2000, which were hailed as a breakthrough and accepted almost universally as the new global care standard. Unfortunately, the quality of care did not follow the accreditation, at least in the US market where TJC has enjoyed a virtual monopoly for over thirty years. Recent reports to this effect include the Commonwealth Report, the VHA scandal and recent DoD revelations, which have a lot of people wondering how fundamental patient care processes could have been missed in the thousands of accreditation surveys conducted over decades in the VHA, DoD (and CMS) Systems. Arguably TJC and JCI are among the best available standards. This leaves us with final questions about why the US is ranked poorly:
a)Â Â Â Â Do other countries have better External Evaluation Mechanisms?
b)Â Â Â Â Do other countries simply follow the standards more closely?
c)Â Â Â Â Do they enforce compliance more rigorously?
d)Â Â Â Â Do they follow better processes and procedures?
e)Â Â Â Â Do they provide more empathetic care?
f)Â Â Â Â Â Â Do they show less concern for the bottom line?
g)Â Â Â Â Do they have better training and education?
h)Â Â Â Â Do they have better equipment and newer technology?
These are not rhetorical questions; they need to be answered to draw reasonable conclusions. In our opinion, the survey can provide some directional input but also has a lot of credibility issues as discussed above, particularly in the methodology and ranking approach. And it should be mentioned that the ultimate measure will be based on (successful) outcomes achieved versus (equitable) resources employed, something the industry will be wrestling to measure accurately for some time to come.
On a final note, as consultants we are always looking for progress in these Environment of Care and Clinical areas, but unfortunately we find from evidence-based reporting that performance is not improving compared to earlier periods despite improved technology,  economic growth and constant tweaking of the standards. Just as important,  at the core of our business is the other set of standards that are critical to the Healthcare Industry and often underappreciated: Safety and Security from Natural and Manmade Events. The world is becoming increasingly dangerous from more frequent and severe natural disasters, more virulent and resistant viruses and biological agents, and the manmade threats of workplace violence, active shooters and terrorist attacks against soft targets like hospitals.





0 Comments