As the VA scandal unfolds and we watch the talking heads go back and forth on how to minimize waiting times and improve continuity of care, the Congress is acting like this is all a big surprise. Watching the CSPAN hearings today and seeing what testimony was encouraged, and what was cut short unceremoniously, particularly several good points by Betsy McCaughey, PhD, make us curious about what the final draft bill will look like. From our perspective there is a big question of intellectual honesty here, and lack of focus on a couple of key issues:
1) Who is responsible for oversight of the VHA system?
2) What sources of information are available to inform this oversight?
 As mentioned in our previous post, Congress is responsible for oversight of the VHA. From field research and working with clients, we know that the Congress receives regular input in the form of complaints by veterans and that Congress passes these complaints on the respective VA Medical Centers. Apparently, the number of these complaints is high and some VA Hospitals get them at the rate of several per month – and that the hospitals accept them as something akin to the “course of doing businessâ€, rather than the escalation of serious issues they should be. This means two things to us:
As mentioned in our previous post, Congress is responsible for oversight of the VHA. From field research and working with clients, we know that the Congress receives regular input in the form of complaints by veterans and that Congress passes these complaints on the respective VA Medical Centers. Apparently, the number of these complaints is high and some VA Hospitals get them at the rate of several per month – and that the hospitals accept them as something akin to the “course of doing businessâ€, rather than the escalation of serious issues they should be. This means two things to us:
a) Â The VHA does not take these escalations seriously enough
b) Congress does not follow up or attempt to solve the issues aggressively enough
Also mentioned in our previous post is the fact that the most comprehensive, expensive and persistent source of information to Congress is the 30 year monopoly granted to The Joint Commission by Congress to conduct Accreditation, Review Quality of care, Consult on Quality of Care, Organization, Leadership, Management of Information, and others. That thousands of surveys could be conducted over the last ten years alone, and missed these administrative and IT issues is almost beyond belief.
Quoting directly from the VHA Handbook:
“TJC has been accrediting VHA facilities for over 30 years. TJC is an internationally accepted external validation that an organization has systems and processes in place to provide safe and quality oriented health care. Compliance with TJC standards and accreditation processes facilitates risk reduction and performance improvement by standardizing critical procedures and processes. Many VA directives and policies provide specific reference to TJC standards and accreditation for specific programs and functions (including, but not limited to, credentialing and privileging, tele-radiology, health information management, environmental management, occupational safety and health, disclosure of adverse events, patient safety, and billing for services).
c. In order to achieve TJC accreditation, VHA medical facility and ambulatory health care systems must focus on:
(1) National Patient Safety Goals.
(2) Patient-Focused Functions, including Ethics; Rights and Responsibilities; Provision of Care, Treatment, and Services; Medication Management; Surveillance, Prevention, and Control of Infection.
(3) Organization Functions, including Improving Organization Performance; Leadership; Management of the Environment of Care; Management of Human Resources; and Management of Information.
(4) Structures with Functions, including Medical Staff and Nursing. VHA Handbook 1100.16 September 22, 2009
(5) Performance Measurement (Process and Outcomes)â€
This Long standing monopoly arrangement has left TJC complacent and riddled with conflicts of interest, making it difficult to press clients into higher levels of performance. VHA has allowed a no-bid award process to continue accreditation in spite of evidence-based failures to protect our veterans.
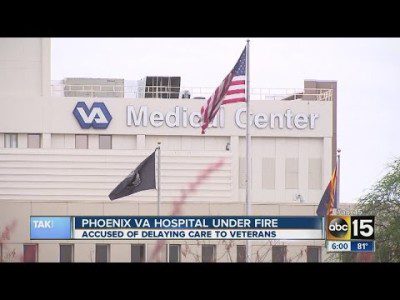
Consider that in the months before the Walter Reed scandal in 2006, the hospital was awarded a 96 percentile report from their TJC Survey, and that the Phoenix VA Med Center, which is at the heart of the current fiasco, was rated by TJC as one of the Top 20 hospitals in the nation for patient safety in 2010.
 While we cannot minimize the role senior management played in missing the warning signs, we do point to General Shinseki’s written testimony to Congress on May 15:
While we cannot minimize the role senior management played in missing the warning signs, we do point to General Shinseki’s written testimony to Congress on May 15:
“Every year, our dedicated VA employees, many of whom are Veterans themselves, provide 6.3 million Veterans with the excellent care they have earned and deserve. VA provides a broad range of primary care, specialty care, and related medical and social support services. We have established a record of safe, exceptional care that is consistently recognized by independent reviews, organizations, and experts on key health care quality measures. Every VA medical facility is accredited by The Joint Commission, the independent, non-profit organization that ensures the quality of U.S. healthcare by its intensive evaluation of more than 20,000 healthcare organizations. In 2012, The Joint Commission, recognized 19 VA hospitals as top performers, and that number increased to 32 in 2013.â€
That VHA  continue not to hold their sole external evaluation mechanism accountable makes us wonder whether to be furious at Congress or applaud the skill of a host of enablers, wittingly and unwittingly employed by TJC, who have done such an excellent job keeping them out of the spotlight. As is so often the case these days, Congress conducts heated hearings to attempt a legislative fix where everybody can get on the record with their feigned outrage, when what is really needed is to enforce the existing laws or determine an effective action-oriented, no excuses method to solve the problem.





0 Comments