We originally published this “Myths and Realities” piece as a letter to ACHE in 2007 and then as a blog post in 2014. Many of our clients would rationalize their lack of preparedness for Terrorist Attacks by claiming their location, geographical circumstances, or membership in a larger consortium made them less vulnerable. That was not, and is not true, as described below:
Myth: Federal terrorism response plans call for immediate assistance to sites of significant terrorist attacks.
Reality: Using Federal grants, Emergency Planning, budgeting, and execution are done at the State and Local levels, and the local area is expected to be able to handle a surge for 72 hours. The National Response Plan, through the National Incident Management System, provides for limited assistance after an initial seventy-two (72) hour surge in demand. Following a significant terrorist event, however, the timeline of federal-level assistance is determined by the nature of the incident, the national security estimates, and federal mission priorities. Multiple incidents may delay federal assistance indefinitely. Even so, Federal response is never quick enough for those on the ground. An organization’s survival depends on its vigilance and application of the Readiness elements of Mitigation, Preparation, Response, and Recovery. FEMA is responsible for helping prepare for disasters by coordinating plans on the front end of disasters; they do not play an active role in responding to the disaster other than helping coordinate Federal, State, and Local resources. Post-Event, they also coordinate Federal assistance, depending on the nature of the event.
Myth: We are a small rural facility and a less likely target.
Reality: Agro-terrorism is a real vulnerability. The first line of defense is the small rural or critical care facilities. Rural areas have the highest probability of receiving “crop duster” attacks, crop dusting being a familiar activity in those areas. Rural facilities are also critical to take the stress off Urban Medical Centers and Suburban Clusters during mass casualty events.
Myth: We are a suburban facility, and the large metropolitan facilities and local governmental planners are preparing for a terrorist response, so the probability of our direct involvement is unlikely.
Reality: Clustered urban healthcare facilities are seen as soft infrastructure targets with a high probability of “dirty bomb” victims. Destruction of these healthcare assets forces care to the beyond suburbs. Whether the medical centers are the primary target or an attack with a high-profile urban target in the vicinity, this strategy is designed to maximize lethality and deny treatment for victims.
Myth: We have not formally participated in local or regional planning or received any federal grant funds for CBRNE Readiness, so we are not obligated to have an emergency management plan that meets NRP/NIMS/ICS expectations.
Reality: Homeland Security Presidential Directives have designated all hospitals as Critical Infrastructure/Key assets and medical staff as First Responders/First Receivers. The DHHS’ Center for Medicare and Medicaid Services (CMS), requires all-hazards (including CBRNE) preparedness as a Condition of Participation (COP) to receive federal dollars for services. Satisfying TJC accreditation standards is insufficient for a robust All-Hazards Emergency Plan.
Myth: Everyone knows that terrorists are looking for spectacular, high victim count, high profile targets. We don’t meet those criteria, so we have little to fear.
Reality: Recent intelligence estimates indicate that the likelihood terrorists would choose one large target has reduced by twenty-five (25%), and the selection of multiple smaller targets has increased, especially regarding critical infrastructure. Target selection is partially a function of access, as larger targets are “hardened”. Selecting “softer,” more vulnerable targets is more likely; bringing down a large Medical Center and nearby hospitals impedes care for a larger area and interferes with contingency plans. Recent Insurance industry target modeling also reflects a shift away from larger targets.
 Myth: Hospitals are unlikely terrorist targets, and if they were selected, it would be large, famous medical centers in urban settings. We don’t fit that description, and it is improbable that a small-town healthcare facility would be targeted.
Myth: Hospitals are unlikely terrorist targets, and if they were selected, it would be large, famous medical centers in urban settings. We don’t fit that description, and it is improbable that a small-town healthcare facility would be targeted.
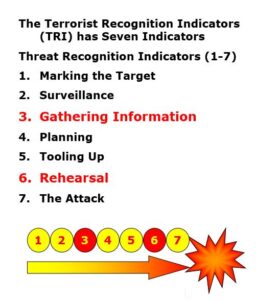
Reality: Recent highly suspicious activities involving fake federal and accrediting hospital inspectors appearing in the middle of the night asking for building tours have little common pattern relative to size, geography, ownership, or specialty. A spate of unexplained intense interest in specific areas of healthcare facilities focused on pharmacy and radiology departments had little in common with facility characteristics. Theft and questionable purchases of used ambulances appear to be geographically random events. The use of vehicles as future terrorist delivery systems is commonly accepted, with VIP limos, mortuary transports and ambulances heading the list. An unsettling aspect associated with false hospital inspectors is predicated on the commonly accepted hierarchy of Terrorist Recognition Indicators (TRI), as seen in the graphic on the left.
Many experts classify Terrorist Recognition Indicators (TRI) along a seven-stage continuum, where it is not clear whether Stage 3, “Gathering Information,” is Stage 6, “Rehearsal,” or if the “Rehearsal” is the actual “Attack”. The acquisition and short-term storage of ambulances would appear to be late-stage. Captured terrorist documents identify hospitals as soft targets, and the recently convicted “Lodi Terrorist” testified to a plot to target hospitals across the nation.
Myth: Hospital personnel, particularly professional staff, are trained to recognize and treat CBRNE-related casualties. Our doctors and nurses are already trained to treat mass casualties of all types. They are too busy to participate in CBRNE education and training exercises. When the time comes, they will know what to do.
Reality: Post 9/11 CBRNE emergency management exercises and their after-action/lessons learned reveal that the lack of CBRNE working knowledge among health professionals was a significant weakness in the system. Each Category of CBRNE has unique characteristics and challenges that can be a specialty unto themselves. The need for health professionals’ involvement in all-hazards planning and their active participation in realistic CBRNE exercises is essential to meet future threats.
Myth: Hospital personnel, at all levels, are willing to actively participate in a real CBRNE hostile environment. Our hospital personnel are willing to place themselves in harm’s way in the event of an actual CBRNE threat environment.
Reality: Recent experience with the SARS threat brings into question the validity of this statement. Incidents of refusal to work in such an environment were not unusual. One state survey revealed that half of physicians and nurses answered NO to a question about their willingness to participate in a real CBRNE event in a non-hospital setting. This is significant because the hospital is on lockdown during many real CBRNE events. There is no substitute for strong leadership, operational training, and understanding of using protective equipment in an actual CBRNE environment for effective, life-saving care and containment.
Myth: The healthcare system has been tested by the Oklahoma City and the 9/11 attacks on New York and the Pentagon. We have sustained terrorist attacks, and we understand a lot more about how to deal with them.
Reality: Although we have gained some insight from those experiences, they were largely mortuary management events. One significant lesson learned was that healthcare facilities were ill-prepared to deal with huge crowds looking for friends and family members. An accompanying biological or chemical attack could have resulted in the immediate contamination of area healthcare resources.
Myth: CBRNE responses differ from those used to deal with natural hazards and the occasional hazmat events. We have been able to deal with multiple catastrophic events, most recently, four major, destructive hurricanes in one season.
Reality: Managing CBRNE risks requires the understanding of significant differences between Natural and man-made terrorist events. To identify a few:
- Predictability
- Casualty production
- The ratio between property loss and loss of life;
- Post-event recovery time;
- Economic impact;
- Public acceptance of the protracted loss of personal freedom and
- the “Terror factor” psychological impact.
Natural hazards are, for the most part, predictable and bounded by geography, for instance, hurricanes. Citizens in Nebraska do not feel anxiety over a Florida hurricane. Terrorist attacks anywhere in the nation create a psychological trauma response in most inhabitants. Katrina may be an exception. Even so, had terrorists planted a couple of “dirty bombs” in the levees or attacked other infrastructure, the entire New Orleans population would have been flooding victims with the added contamination hazard to prevent a timely or effective rescue.
Myth: Our long experience with natural hazards has allowed us to incrementally improve on mitigation, preparation, response, and recovery, giving us comfort in our ability to deal with future events. We have, through trial and error, been able to deal with All Hazards Events.
Reality: Expected new strategies from the terrorist community will test our creativity and resolve. Look and prepare for new terrorist tactics: Planning CBRNE attacks to coincide with predictable natural hazard events, hurricanes as they make landfall; peak flood levels; immediately following earthquakes or coinciding with aftershocks; introduction of different biological agents following Katrina or at peak known endemic or pandemic events; introduction of chemical agents to co-mingle with smoke from forest fires; and others.
Myth: Deciding to ” protect in place or evacuate ” in a CBRNE terrorist event is about the same as preparing for a category three hurricane. We do that almost every year.
Reality: In the case of a hurricane, you have the advantage of knowing hour by hour the location, velocity, and direction of this hazard. There are essentially two elements to deal with: wind and water. The failure of the New Orleans Healthcare Community to be prepared to evacuate or protect in place is testimony to a systems breakdown at all levels of leadership and oversight. The decision window time is short when dealing with an unanticipated chemical or biological agent attack. Agent identification and knowledge of its characteristics, wind speed, and direction, the concentration of the agent, structural integrity of the building, which exit routes are clear, and other information are necessary for action. If the decision is made to” protect in place,” depending on the agent, there are multiple variables to consider, do you go to the top floor or to the basement? Who receives the limited amount of protective equipment? A “to evacuate” decision is no less complex. You get the picture. Remember how a few envelopes of Anthrax powder shut down the USPS and Congressional Office Buildings for weeks in 2001?
Conclusion
The Nation’s twenty-first century is poised with the possibilities of unimaginable advances in our capability to make our citizens healthier and longer-lived. Shadowing that optimistic environment are criminal and sinister forces dedicated to destroying that vision. Protection of the nation’s healthcare infrastructure and the future health and safety of all healthcare industry stakeholders is daunting. The National Response Plan, through implementing the National Incident Management System, provides the industry with an integrated framework and process to meet future terrorist threats effectively. The greater healthcare industry must adopt a proactive posture of meeting NRP expectations. An important step in the process is for the industry to adopt an “intellectually honest” attitude in the HVA process. Hospitals find themselves in the unique position of having the timely and critical mission of treating victims of terrorist attacks and the additional duty of protecting patients, employees, visitors, vendors, and valuable research experiments. Expert congressional testimony indicates that the threat is real and is “not if, but when”. Mounting evidence points to a special interest by terrorists in healthcare facilities as future targets. This interest is wide-ranging, selecting potential targets without regard to geographic location, size, ownership, or specialty care.
Over the past fifty years, the hospital industry has adjusted to progressively more demanding all-hazards requirements. Recent history shows us that the system, with few exceptions, has effectively dealt with non-terrorist all-hazards events. Most of the nation’s hospitals possess documented evidence through government or private accrediting mechanisms that they are prepared to deal with the HSPD’s definition of all-hazards events. Observers from all quarters question the healthcare industry’s preparedness to meet the terrorist challenge.
The hospital industry is not alone in the private and public sectors in the apparent lack of zeal to voluntarily comply with NRP readiness expectations. Recent Congressional and media speculations that DHS will need to move to federal mandates for compliance have not missed the attention of leadership in these sectors. Delaying action until there is “proof”, of a significant hospital terrorist attack would be a cost the industry can ill afford.
REFERENCES for the letter to the Incoming ACHE Chairman sent in 2007.
- Report of National Commission on Terrorist Attacks upon the United States, Official Government Edition. The commission established by Title VI of Public Law 107-306, 107th Congress, 2nd Session, November 27, 2002, was made public on July 22, 2004.
- Homeland Security Act of 2002, Public Law 107-296 (November 25, 2003).
- (a) Trust for America’s Health Reports, Ready or Not? Protecting the Public’s Health in an Age of Bioterrorism, December 2004, 2005.
(b)Haase, L.W., Breathing Easier? Â Report of the Century Foundation Working Group on Bioterrorism Preparedness, January 13, 2003.
(c) Gursky, E.A., ScD., Senior Fellow for Biodefense and Public Health ANSER Institute for Homeland Security. Hometown Hospitals: The Weakest Link? Bioterrorism Readiness in America’s Rural Hospitals.A Report Commissioned by the National Defense University, Center for Technology and National Security Policy, June 2004.
(d) Rubin, J.N., Recurring Pitfalls in Hospital Preparedness and Response, Journal of Homeland Security, January 2004.
(e) Alderidge, J. and Launt, P., Are Hospitals Our Weakest Link?, Access Control and Security Systems, August 1, 2004.
(f) Mayors release New Homeland Security Survey at 72nd Winter Meeting of the U.S. Conference of Mayors, Press release The United States Conference of Mayors, January 22, 2004 pp 1-3.
(g) Santora, M., New York Hospitals See Lack of Preparedness for Disaster, New York Times, August 26, 2004.
(h) Nintz, J. and Warrick, J., U.S. Unprepared Despite Progress, Experts Say, Washington Post, November 8, 2004.
(i) Barbera, J.A., M.D., Macentyre, A.G., M.D., and DeAtley, C., PA-C, How to Forecast The Next Waves of Catastrophic Terrorism, Ambulances to Nowhere: America’s Critical Shortfall in Medical Preparedness for Catastrophic Terrorism? , Journal of Homeland Security, March 2002.
- (a) Most Urban Hospitals Have Emergency Plans but Lack Certain Capacities for Bioterrorism Response, GAO-03-924, August 2003.
(b) Bioterrorism: Preparedness Varied across State and Local Jurisdictions. GAO-03-373, April 7, 2003.
(c) HHS Bioterrorism Preparedness Programs: States Reported Progress but Fall Short of Program Goals for 2002, GAO-04-360R February 10, 2004.
(d) HHS, OIG, Nationwide Audit of State and Local Governments Efforts to Record and Monitor Sub-recipients’ Use of Bioterrorism Hospital Preparedness Program Funds, (A-05-04-00028) August 26, 2004.
- National Response Plan, Appendix 3, Authorities and References, pp. 78-84. December 2004.
- Final 9/11 Commission Report, Commission Recommendations (see reference #1).
- Serio, G.V., New York State Superintendent of Insurance, Testimony before the U.S. House of Representatives Subcommittee on Capital Markets, Insurance, and Government Sponsored Enterprises and Subcommittee on Oversight and Investigations, April 28, 2004 pp 1-24.
- US terrorism insurance: continuing protection. Acts of terrorism in the US may become uninsurable if the government does not renew TRIA. Insurance Business Review, December 17, 2004, Source: Datamonitor Commentwire.
- Baily, D., Emergency Preparedness: D&O Lessons from September 11, PLUS, Professional Liability Underwriters Society, Journal Article June 2002-Volume XV, Number 6.
(a) Savage, C., US Sees Insurers as Possible Tool in Terror Fight, Boston Globe, February 22, 2005.
(b) Ramstack, T. Insurance Discounts Eyed for Security, Washington Times, March 07, 2005.
- Decker, R.J., Director Defense Capabilities and Management, Homeland Security: Key Elements of a Risk Management Approach, Testimony before the Subcommittee on National Security, Veterans Affairs, and International Relations; House Committee on Government Reform, October 12, 2001, GAO-02-150T.
- The National Strategy for Physical Protection of Critical Infrastructure and Key Assets, Public Health and Emergency Services, PP, 41-44. The White House Feb. 2003.
- Barbisch, D., DHA and McGlown, J.K., PhD., R.N., CHE, presentation,
Coordinating Civilian and Military Disaster Response, Seminar 34, American College of Healthcare Executives, 2005 Congress on Healthcare Management, March 15, 2005
(see 3, i).
- National Response Plan: Homeland Security Implementation Guidance pp. ix-xiii, December 2004, Released to the public January 6, 2005.
- (Senate Bill: S. 2845, Section 7305, Private Sector Preparedness) Congressional Record December 7, 2004, H10930-H10993 Conference Report on S. 2845, Intelligence Reform and Terrorism Prevention Act of 2004.
- Belmont, E., Esquire; Fried, B.M., Esquire; Gonen, J.S., Esquire; Murphy, A.M., Esquire; Sconyers, J.M., Esquire; and Zinder, S.F., Esquire,
- The Emergency Preparedness, Response, and Recovery Checklist: Beyond the Emergency Management Plan, American Health Lawyers Association, 2004, pp. 1-38.
- Lanzilotti, S.S.; Galanis, D.; Leoni, N.; and Craig, B., 2002 “Hawaii Medical Professionals Assessment: A Study of the Availability of Doctors and Nurses to Staff Non-Hospital Field Medical Facilities for Mass Casualty Incidents Resulting from the Use of Weapons of Mass Destruction and the Level of Knowledge and Skills of These Medical Professionals as Related to the Treatment of Victims of Such Incidents.” Hawaii Medical Journal 61 (8): 162-74.
- Kephart, J.L. 2005 “Immigration and Terrorism: Beyond the 9/11 Report” CIS.org, September 30. 2005
- Department of Health and Human Services, Guidance for Protecting Building Environments from Airborne Chemical, Biological, or Radiological Attack, Washington D.C. : National Institute for Occupational Safety and Health, May 2002 (NIOSH Pub. No. 2003-139)
- Department of Homeland Security, Interim National Infrastructure Protection Plan, Washington D.C.: February 2005
- National Infrastructure Protection Center, “Risk Management: An Essential Guide to Protecting Critical Assets,” Washington D.C., November 2002.
- White House -2003, National Strategy for the Physical Protection of Critical Facilities and Key Assets, Washington D.C. February 2003
- American College of Emergency Physicians, “National Report Card on the State of Emergency Medicine” ACEP, Jan 2006
- Lee, G. C., Sternberg E., “Meeting the Challenge of Facility Protection for Homeland Security,” Journal of Homeland Security and Emergency Management, Volume3, Issue 1, Article 11, 2006
- Flynn, S.E., Prieto, D.B., Mobilizing the Private Sector to Support Homeland Security, CRS No. 13, Council on Foreign Relations, March 2006
- GAO-03-315R, Homeland Security: CDC’s Select Agency Program, November 22, 2002.
- GAO-06-442R, Hurricane Katrina
- GAO-06-365R, Preliminary Observations on Preparation, Response, Katrina
- GAO-01-4, Influenza Pandemic: Plans needed for Federal and State Response, October, 2000.
- Smith J.L., Anti-Terrorism: Criteria, Tools, and Technology, Applied Research Inc., Feb. 2003
- Mantone, J., The Big Bang: The Hill-Burton act put hospitals in thousands of ….., Modern Healthcare, August 15, 2005
- Sloan, T., Still not ready, Healthcare’s front-line responders unprepared for most-likely terrorist threat, Modern Healthcare, August 29, 20
- Blair, J., What about terrorism? Opinions Letters, Modern Healthcare, August 29, 2005
- Meyers, R., General (Ret) Chairman of the Joint Chiefs of Staff, Code Red, The Reality of Risk, Healthcare in Crises Mode, Medical News, Jan. 2006, KY Medical news(KY, OH, IN)
- Abbott, E.B., Hetzel, O.J., Editors, A Legal Guide to Homeland Security and Emergency Management for State and Local Governments. ABA, 2005.
- ABA, Center for Continuing Education, DVD, Are you ready? What Lawyers Need to Know About Emergency Preparedness and Disaster Recovery, 2005
- Tierney, K.J., Lindell. M.K. Perry R.W., Facing the Unexpected: Disaster Preparedness and Response in the United States, Washington D.C., John Henry Press, 2001
- Simon., ” Spotlight on Security.” Liability Reports, January 2002
- National Research Council, Protecting People and Buildings from Terrorism: Technology Transfer for Blast-effects Mitigation, Washington D.C.: National Academy Press, 2001
- Voeller, J.E., “CIPP: Critical Infrastructures Protection Priorities” Construction Sciences Research Foundation, August 2003
My Recent Publications on the Issues
Unpublished Manuscript Title:
- Pre-Katrina: U. S. NON-FEDERAL HOSPITAL INDUSTRY vs HOMELAND SECURITY CBRNE READINESS”
- Post Katrina/New Orleans U. S. NON-FEDERAL HOSPITAL INDUSTRY vs. HOMELAND SECURITY ALL HAZARDS READINESS”
- Current working Title: “Homeland Security and Healthcare –A Tale of Apathy, Denial, or Worse?â€
Recent publications which deal with Homeland Security CBRNE and All-Hazards Healthcare Readiness:
- Blair, J.D., All-Hazards “HVA” for Non-Federal Healthcare CBRNE Readiness: A Level Playing Field? Inside Homeland Security, Volume 3, Issue 5, Sept/Oct 2005.
- Blair, J.D., Homeland Security, and the Non-Federal Healthcare Sector: evaluation of your Incident Command System (ICS), Journal of Healthcare Protection Management, Volume 21 Number 2, Summer 2005.
- Blair, J.D., Homeland Security, and Non-Federal Health Sector: Incident Command Structure. Hospital Fire Marshal’s News (HFMA), April 2005
- Blair, J.D., National Response Plan and the Non-Federal Healthcare Industry’s Design and Construction Community, MATRIX, 2005
- Blair, J.D., Healthcare Readiness for CBRNE Terrorist Events, Emergency Response Manual, Chapter 25, Anti-Terrorism Board Certified Anti-Terrorism Specialist (ATAB)
- Blair, J.D., Edwards J. T., Homeland Security and the Non-Federal Sector Readiness: A Risk Management Challenge? Journal of Healthcare Risk Management, October 2005
- Blair, J.D. Is Healthcare the Weak Link in the Homeland Security Chain? MEDICAL News, January 2006, KY Medical News(KY,IN , OH)
- Blair, J.D., Homeland Security and the Non-Federal Sector Readiness. Hospital Fire Marshal’s Association, Part 1, December 2005, Part 2, January 2006.
- Blair, J. D., Is The Healthcare Industry Prepared for Terrorism? Journal of Healthcare PROTECTION Management, Volume 22, Number 1,
- Blair, J.D., Silver, R. B., Modern Healthcare, “Commentary” Daily Dose and Modern Healthcare online, January 2007.
- Blair, . D., Scanlon, P. A., Pandemic Flu Threat and Business Continuity. Elliot Consulting Group, News Letter,
- Blair, J. D., Dluzneski, P. K., Evolving Roles and Responsibilities for Healthcare Security Professionals: The Non-Federal Healthcare Sector Meets NIMS and NIPP, Journal of Healthcare PROTECTION Management, January 2007.
- Blair, J. D., NIPPS vs Non-Federal Hospital Design and Construction, letter to the editor, Health Affairs, July 2006.
- Blair, J. D., â€Lagging Healthcare Sectorâ€, Updates and Responses, HSToday, April 2007.




0 Comments