This is the second in a three part series on how Accreditation in Healthcare has failed to keep us safe from the threats of  more frequent and robust natural disasters, more virulent and drug-resistant biological agents, and increasing levels of man-made violence in healthcare, including active shooters, terrorist threats and workplace violence. The first post in this series examined the clinical side of safety and security, this one will focus on natural disasters and biological agents, and the following post will look at violence in the healthcare setting and summarize the inability of the Accreditation process in general and TJC in particular, to check the rise of preventable hospital deaths and injuries.
To Treat and Cure Them, You Must First Keep Them Safe
None of these issues are new; we have been raising them to those leaders who should be providing appropriate oversight in the Public Health and Healthcare sector.  The other side of safety and security involves keeping the patients, staff and visitors safe from Natural and Man-made Disasters (All Hazards Events). We live in an era of increasing uncertainty and danger from more frequent and robust natural disasters, more virulent and drug resistant biological agents, and increasing threats of internal and external violence.
Natural Disasters:
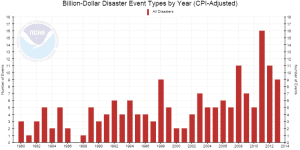 According to this good NOAA Interactive Tool, the number of billion-dollar weather related events in the last 35 years has grown from a low of 0 in 1987 to a high of  16 in 2012.Examples of healthcare failures to protect stakeholders these are legion; Katrina was the worst in our history with over 300 inpatient lives lost from preventable causes, such as lack of electricity to maintain air conditioning and life-sustaining medical equipment  due to flooding of primary and back-up generators that were below the flood plain. A recent TJC Online Report provided an overview of the most challenging Accreditation and Certification Requirements for the first half of 2014. According to the report:
According to this good NOAA Interactive Tool, the number of billion-dollar weather related events in the last 35 years has grown from a low of 0 in 1987 to a high of  16 in 2012.Examples of healthcare failures to protect stakeholders these are legion; Katrina was the worst in our history with over 300 inpatient lives lost from preventable causes, such as lack of electricity to maintain air conditioning and life-sustaining medical equipment  due to flooding of primary and back-up generators that were below the flood plain. A recent TJC Online Report provided an overview of the most challenging Accreditation and Certification Requirements for the first half of 2014. According to the report:
“The Joint Commission collects data on organizations’ compliance with standards, National Patient Safety Goals (NPSGs), the Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgeryâ„¢, and Accreditation and Certification Participation Requirements to identify trends and focus education on challenging requirements. These data also help The Joint Commission identify risk areas to highlight in the Focused Standards Assessment (FSA) process.â€
Among the findings in the report related to hospital readiness to address emergency requirements associated with these increasing Natural Disasters, there was a whopping 58% non-compliance rate for “Manages Risks Associates with Utility Systems” within Critical Access Hospitals, while within Hospitals the non-compliance rate was 53%. These numbers underscore the problem and beg more urgent action on the remediation of these deficiencies. We would suggest much more aggressive oversight in these areas. And some sunshine; no doubt many of these hospitals will show up in the “Best Hospital Rankings†lists that are published in the popular press.
 Despite high levels of self-reported Emergency Management readiness at the State and Local levels in Joplin, Mo., after-action reporting showed that Long Term Care providers were not invited into the Community Disaster Management Planning Process. Â In the massive 2011 Joplin tornado disaster, 11 residents of a single long term care facility lost their lives.
Despite high levels of self-reported Emergency Management readiness at the State and Local levels in Joplin, Mo., after-action reporting showed that Long Term Care providers were not invited into the Community Disaster Management Planning Process. Â In the massive 2011 Joplin tornado disaster, 11 residents of a single long term care facility lost their lives.
In a scathing OIG Report released in September 2014 concerning the preparation and response to Hurricane Sandy, results showed that 89% of the hospitals surveyed reported “Critical Challenges†such as electrical and communications failures and that most had been cited for three years before the storm. Half experienced electrical failures, the cause of hundreds of lives lost seven years earlier during Hurricane Katrina exact same problems for nurses, including lack of training to manually operate automated IV drips and respirators when machines lose power.
It seems the only consequences for not fixing the deficiencies was another round of billions in taxpayer dollars to repair the hospitals, and a lot of backslapping about how well hospitals responded to the crisis. One of the evacuated hospitals that flooded out and had to be evacuated, Langone, was advertising itself as one of the safest hospitals in the country within months of reopening. Â If the hospitals were accredited and cited for being uncompliant in Emergency Management, for the exact reasons that caused the failures, what is the purpose of Accreditation, and where is the accountability?
 Despite the claims that there were no healthcare-related deaths as a result of the storm, a study of 610 long term care (LTC) residents from a Sea Crest Nursing Home in Brooklyn revealed that within three months of evacuation 125 had died. These were a fraction of the 5,500 LTC and Adult Home residents evacuated during the storm. In addition to the Tornadoes, Flooding and Super storms, Drought, Ice Storms and Wildfires have become increasingly prevalent in the last decade due to climate change.
Despite the claims that there were no healthcare-related deaths as a result of the storm, a study of 610 long term care (LTC) residents from a Sea Crest Nursing Home in Brooklyn revealed that within three months of evacuation 125 had died. These were a fraction of the 5,500 LTC and Adult Home residents evacuated during the storm. In addition to the Tornadoes, Flooding and Super storms, Drought, Ice Storms and Wildfires have become increasingly prevalent in the last decade due to climate change.
The healthcare industry’s “sicker and quicker” approach to admit and keep acute cases while discharging them as soon as it is safe, exacerbates this danger of the disasters; more fragile patients in the ICU and NICU are likely to need evacuation in the worst case scenario, and these patient rely most on life-sustaining equipment, driving  the need for adequate electricity, food, water and medicine during emergencies. The most fragile patients were the ones evacuated down dark, flooding staircases during Sandy. Although none have officially been counted among the fatalities from the storm, a follow up of those patients might reveal higher morbidity or worse outcomes than others, especially among the elderly.
Â
Increasingly Virulent Bio-Agents:
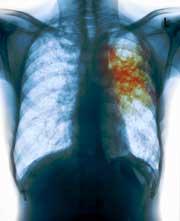 Many experts believe the greatest threat to the human race is the possibility of a global pandemic sweeping across borders faster than it can be contained. More virulent and drug resistant biological agents are proliferating around the globe and are able to move quicker than ever before with the billions of international travelers. H1N1, H5N3, SARS, MERS, HEV68, Marburg, and Drug-resistant TB have all emerged as international threats within the past few years. MERS is an airborne disease that continues to spread rapidly as pilgrims fly in and out of Saudi Arabia, with deaths increasing from 302 to 318 between the 13th and 25th of September.
Many experts believe the greatest threat to the human race is the possibility of a global pandemic sweeping across borders faster than it can be contained. More virulent and drug resistant biological agents are proliferating around the globe and are able to move quicker than ever before with the billions of international travelers. H1N1, H5N3, SARS, MERS, HEV68, Marburg, and Drug-resistant TB have all emerged as international threats within the past few years. MERS is an airborne disease that continues to spread rapidly as pilgrims fly in and out of Saudi Arabia, with deaths increasing from 302 to 318 between the 13th and 25th of September.
The US is seeing a resurgence of measles, a disease that was essentially eradicated with the help of strong Public Health programs to vaccinate children. The 2009 H1N1 response was completely inadequate in containing the spread, and the latest OIG report concerning Epidemic Influenza Preparedness is titled: “DHS Has Not Effectively Managed Pandemic Personal Protective Equipment and Antiviral Medical Countermeasures“. Major findings include that the national stockpile of 200,000 respirators to be distributed in a pandemic have exceeded their warranty dates, as has all the hand sanitizer and a majority of the anti-viral vaccines and medications. As seen in this Frontline slide Show, the growing number and types of drug resistant bacteria is alarming, as is the loss of efficacy in existing antibiotics and lack of new antibiotic drugs in the pipeline. For a deeper look at this serious public health issue see the VIDEO. It shows how NIH brought a drug-resistant-bacteria into their premier hospital and were unable to control it or eradicate it from the premises. As we address the challenge of Ebola inside our borders we need to keep in mind that the NIH and CDC are our main line of defense and they are already stressed to capacity dealing with these other challenges.
 The 2014 EBOLA crisis will certainly bring more of the virus to the United States with the deployment of thousands of troops, and according to Reuters, Emory University had serious issues dealing with the hazardous waste associated with treatment of the two Ebola patients they treated. The report said their HAZMAT waste partner refused to handle the material and a deal had to be brokered by CDC and the waste disposal contractor as infectious waste piled up for six days inside the hospital. This is an excellent example of how even the most “ready” facility in the country can be vulnerable to unforeseen and unplanned difficulties. From an accreditation perspective, the above mentioned TJC Online Report, 42% of Critical Access Hospitals and 50% of Hospitals are non-compliant in the area of “Reduces the risk of infections associated with medical equipment, devices, and supplies”.  This begs the question of whether the hospitals which failed are still operating and treating patients with public money; we know it is extremely rare for a hospital to lose their Accreditation and Certification as the result of poor performance in an Accreditation survey. As if these numbers were not alarming enough, Infection Control Today release d results of a survey that says Registered Nurses overwhelmingly believe we are unprepared to treat Ebola. Key Findings:
The 2014 EBOLA crisis will certainly bring more of the virus to the United States with the deployment of thousands of troops, and according to Reuters, Emory University had serious issues dealing with the hazardous waste associated with treatment of the two Ebola patients they treated. The report said their HAZMAT waste partner refused to handle the material and a deal had to be brokered by CDC and the waste disposal contractor as infectious waste piled up for six days inside the hospital. This is an excellent example of how even the most “ready” facility in the country can be vulnerable to unforeseen and unplanned difficulties. From an accreditation perspective, the above mentioned TJC Online Report, 42% of Critical Access Hospitals and 50% of Hospitals are non-compliant in the area of “Reduces the risk of infections associated with medical equipment, devices, and supplies”.  This begs the question of whether the hospitals which failed are still operating and treating patients with public money; we know it is extremely rare for a hospital to lose their Accreditation and Certification as the result of poor performance in an Accreditation survey. As if these numbers were not alarming enough, Infection Control Today release d results of a survey that says Registered Nurses overwhelmingly believe we are unprepared to treat Ebola. Key Findings:
- More than 60 percent of RNs say their hospital is not prepared for the Ebola virus.
- 80 percent say their hospital has not communicated to them any policy regarding potential admission of patients infected by Ebola
- 85 percent say their hospital has not provided education on Ebola
- 30 percent say their hospital has insufficient supplies of eye protection (face shields or side shields with goggles) and fluid resistant gowns
- 65 percent say their hospital fails to reduce the number of patients they must care for to accommodate caring for an “isolation†patientâ€
As with lack of preparedness for Natural disasters, without serious consequences or accountability for that kind of performance, we will not be ready to deal with a large scale epidemic regardless of what officials say to the contrary.
As mentioned earlier, our next post will examine internal and external violence in the Healthcare industry.






0 Comments