We originally published this article in Journal of Healthcare Protection Management, volume 28, #1, in early 2012. Many of the same issues exist today and some have become worse, as noted at the end of the article.
Drugs, drugs – who has the drugs?
Dr. James Blair, DPA, MHA, FACHE, FABCHS, MCASÂ
Drug diversion, although on the increase, is not the only problem involving drugs that hospital security officials should be concerned with. Growing drug shortages, off-shore production, counterfeiting, and weaknesses in the drug supply chain in case of a world-wide pandemic, are even greater causes for concern, the author claims.
(Dr. James Blair, DPA, MHA, FACHE, FABCHS, MCAS is president and CEO of the Center for Healthcare Emergency Readiness (CHCER), Nashville, TN.)
Recent reports about hospitals experiencing shortages of critical life-saving drugs should command the attention of those who provide physical safety and security to those organizations. Media accounts of shortage of this or that drug rarely cause a blip on the screen. A recent article dealing with a shortage of drugs for the execution of some vicious killer received a lot of press and excited pro and anti- death adherents. Few questions surfaced about why there was a shortage of the drug or how we could find a solution to the problem.
THE GROWING SHORTAGE OF CRITICAL DRUGS
A record number of drugs are in short supply nationwide, the Long Island, New York newspaper Newsday reported — a crisis that is being felt by local hospitals as they scramble to find medicines for patients facing serious medical conditions. The bulk of the shortage involved generic, injectable drugs used in hospitals and clinics. More than 180 medications — from those treating cancer and childhood leukemia to surgical anesthetics and painkillers — have appeared on the U.S. Food and Drug Administration’s list of critical shortages this year.
 In the past five years, the FDA’s list of drugs in short supply has nearly tripled, up to 178 last year from 61 in 2005. More than half of the recent shortages are due to government inspectors finding contamination problems in drug plants in the United States and abroad, stopping production, the newspaper found. Plant closures in the United States, and a lack of raw materials, also have contributed to the shortages.
In the past five years, the FDA’s list of drugs in short supply has nearly tripled, up to 178 last year from 61 in 2005. More than half of the recent shortages are due to government inspectors finding contamination problems in drug plants in the United States and abroad, stopping production, the newspaper found. Plant closures in the United States, and a lack of raw materials, also have contributed to the shortages.
“The problem has prompted hospital, pharmacy and physician groups across the country to call on the government to step in. One proposed solution: creation of a national stockpile of critically needed drugs.”
WEAKNESSES IN THE DRUG SUPPLY CHAIN
There is no national stockpile of critically needed drugs. The practice of “just-in-time†deliveries has its economic advantages’, it also has its unintended perils. We have followed the evolution of the “Strategic National Stockpile†(SNS). We have also witnessed the dismembering of the nation’s Military Medical Depot System designed to provide available stockpiles of all manner of medical supplies and equipment in the event of hostile actions against the country. Experts tell us that this has seriously weakened our capacity to respond to both military requirements and expected civil support actions during national disasters.
THE INCREASE IN DRUG DIVERSION
Hospitals, clinics and office-based physician practices are seeing an increase in criminal activity (euphemistically called diversion). Drug addiction among healthcare professionals and others employed in health care settings have remained at a steady 10-15 percent over the years; however the diversion of certain drugs has increased dramatically.
For example, according to Health Canada, more than 300 incidents were reported in 2010 by hospitals of drugs that were stolen, pilfered, lost in transit, or were unaccounted for. Losses ranged from a single tablet to thousands of pills and narcotic vials. Some examples of drug diversion included:
Narcotics stored in automated dispensing cabinets in the emergency department of an Ontario hospital accessed only by nursing and pharmacy staff that were reported stolen over a one-year period included 3,007 Oxycontin, 2,268 Oxycodone, 516 Oxycocet, 39 morphine and 28 hydromorphine. A health practitioner said that opiate addiction has climbed, especially in Ontario with the introduction of Oxycontin to the Ontario Drug Benefits Plan
Oxycodone was also the main target of a reported prescription drug operation which led to the arrest of 21 persons, employees and patients, at the West Palm Beach Veterans Affairs Medical Center. Undercover agents said they were able to buy prescription drugs, largely Oxycodone, from hospital staffers as well as veterans who sold their own medication. Some 6,000 Oxycodone pills, two vehicles and $200,000 in cash were seized.
Drug diversion for personal use is troublesome in that it impacts on patient care in a number of ways. Impaired physicians are an obvious hazard to their patients. Caregivers who divert drugs from their patients for personal use pose a real threat to their patient’s course of treatment. This problem is sensitive to “supply and demand†and population behavior. Recent demand has been driven by increases in abuse of prescription drugs and profitability associated with the trade. Diversion is indeed a troublesome issue but it does not pose the major threat to the healthcare system.
THE MAJOR THREAT–OFF-SHORE DRUG MANUFACTURINGÂ
The major threat comes from the escalating off-shore manufacturing of the bulk of formulary medications, those used by all sectors of the nation’s day-to-day healthcare delivery system.
The sobering fact is that two-thirds of the world’s supplies of aspirin are manufactured in China, a real headache if the supply chain is interrupted for any reason.  Seventy percent of the world’s penicillin comes from the same source. The vast majority of medical supplies and equipment are manufactured off-shore.
These locations are subject to the same threats we face in the United States. The triple threats of: Evolving Infectious Diseases; More Frequent and Robust Natural Disasters and Terrorists Attacks haunt all corners of the globe.
CONSEQUENCES OF A WORLD-WIDE PANDEMIC
A virulent world-wide pandemic could compromise the supply chain for disease specific medications, equipment and supplies. The likelihood that off–shore sources would take care of their own populations before exporting limited life-saving materials to others is a reality.
Recent observations of public reaction to a potential Anthrax attack should serve as a reminder to all that the “worried well†posed an imminent threat to hospitals in the nation’s capital. There were rumors that hospital staff had depleted the limited supply of life-saving drugs by hoarding and distributing the drugs to their families and friends enraged the surrounding communities. The healthcare organizations had to lock down their operations and denied them the opportunity to exercise a reasonable response, if they had such a plan.
How hospital boards and C-suites deal with this reality is largely a matter of leadership. We have seen little appetite to move from or moderate the “just in time†paradigm. The industry’s propensity for reactive behavior will probably lead to a last minute scramble for disappearing materials.
The organization’s Safety and Security, Public Safety functions will have the heavy burden of protecting resources in such hostile environments. The Class-Warfare, Civil Disorder we witness in the United Kingdom will be tame compared to roving mobs of citizens vying for life-saving medicines for themselves and their families.
Leadership will have limited choices in an environment of acute shortages of commonly used drugs. Situational awareness will be “king.†Some will moderate their “just in time†protocols by making timely decisions on where and what to stock above current consumption. Making the correct choices may mean the difference between institutional survival and its alternative. Securing and transporting these items becomes the lifeline to survival.
THE MOST SINISTER THREAT–COUNTERFEIT DRUGS
The most sinister of these threats is the likelihood of increased activity in the counterfeit market. Experts tell us that extant screening processes have spared us from any meaningful volume of these fake drugs infiltrating the nation’s drug market. Some think that generic drugs are passing as brand names with marginal harm to patient populations. The same is obviously not the case with fake drugs.
The specter of one 90-day supply of an altered medication given to a patient who is on three or four prescription drugs could well be fatal. Many elderly patients with co-morbidities end up taking drug which are needed for the side-effects of other drugs-on and on. Domestic drug manufactures have had their quality control problems. Off-shore drugs may pass through multiple dealers before reaching the consuming public. Each of those levels provides opportunities to increase their profits through some type of manipulation of quality, which could have deadly consequences for the trusting public.
Vigilance is needed from all who work in healthcare facilities. This is an added burden placed on pharmacy and hospital security personnel.
UPDATE FEBRUARY 2014, TWO YEARS ON…
As reported in the New York Times, the shortage of drugs is trending upwards with increasing danger to patients:
“Despite efforts by the Obama administration to ease shortages of critical drugs, shortfalls have persisted, forcing doctors to resort to rationing in some cases or to scramble for alternatives, a government watchdog agency said on Monday. The number of annual drug shortages — both new and continuing ones — nearly tripled from 2007 to 2012.â€
The article cites the shortages are driven by several factors including price pressure on manufacturers who are using aging production facilities, and need to balance investment with return, along with changes in Medicare reimbursement policies that continue to push prices down –and finally, also vendor concentration which has resulted in over 70% share of products in the sterile injectable cancer category coming from only three vendors, making the market even potentially more volatile.
For a shocking account about the path where the price of a drug goes from $7 to $600 by passing through several intermediaries in the distribution chain, there is this Congressional Report on the gray market.
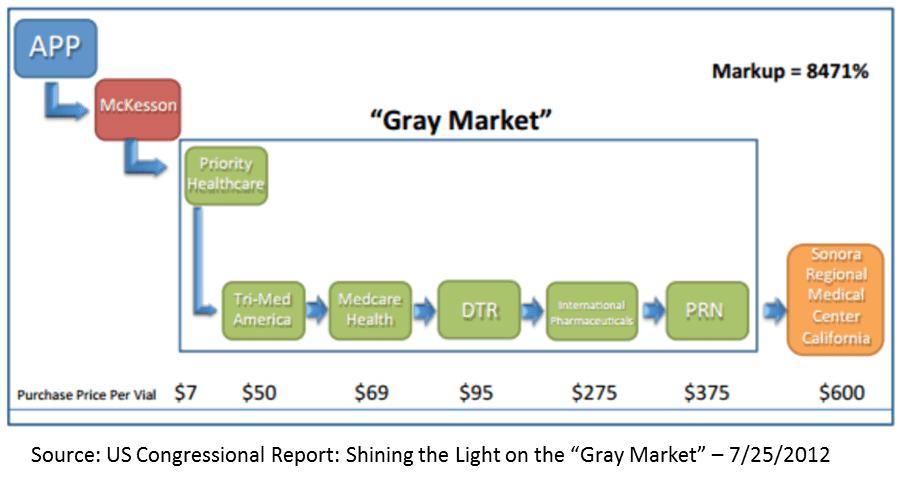 Among the other findings on how manufactured “shortages†are created through profiteering in the supply chain include:
Among the other findings on how manufactured “shortages†are created through profiteering in the supply chain include:
“Fake Pharmacies†Acquire Prescription Drugs from Authorized Distributors and then Sell Them Into the Gray Market. The investigation has identified a number of businesses holding pharmacy licenses that do not dispense drugs, but instead appear to operate for the sole purpose of acquiring short-supply drugs that can be sold into the gray market.Â
“Drug Brokers†Recruit Pharmacies to Purchase Drugs for the Gray Market.
Some gray market wholesalers gain access to shortage drugs by recruiting pharmacies to act as their purchasing agents.
Gray Market Business Practices Are Widespread. Pedigree and price information collected for five different short-supply injectable drugs, documenting the activities of 125 different companies, showed similar patterns of leakage and aggressive gray market price markups. For all five drugs, units normally costing $10 to $20 were regularly marked up to prices of $200 or more while they traveled through the gray market.
Gray Market Drugs Are Marked Up as They Quickly Pass from Owner to Owner. On average, the prescription drugs examined in this investigation were owned by three to four different gray market businesses before being sold to a hospital; most of the drugs traveled through the gray market in five days or less.
Gray Market Companies Sometimes Charge Hospitals Significantly Different Prices for the Same Drug Product on the Same Day. Gray market companies sold units of the exact same drug product to different hospitals on the same day at significantly different prices. On the same day, for example, a gray market company sold a drug to a U.S. military hospital for $315 per unit, and sold the exact same drug product to another hospital for $215 per unit.
Perhaps the most shocking of all is that this activity is legal and although Congress can spend tax dollars on uncovering the problem, there is little appetite for solving it.





0 Comments