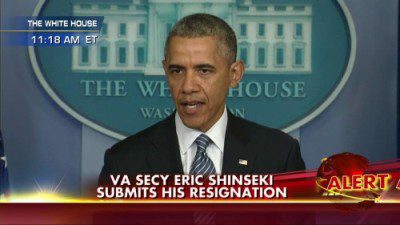
Veterans Administration Secretary General Shinseki resigned his position Friday after a meeting with the President, according to this Washington Post report, falling on his sword to eliminate distractions as the VA scrambles to fix widespread failures to provide timely care to veterans.
 With the hindsight of being an old soldier who has been deeply involved with the DoD and VHA healthcare systems for over forty years, both as a senior DoD Healthcare Administrator and a Combat-Wounded veteran, the recent scandal does not really come as a surprise; there were many warning signs over the past ten years. It was a surprise that those at the top of the organization could be unaware of the long-standing problems that so many veterans face getting access to continued care.
With the hindsight of being an old soldier who has been deeply involved with the DoD and VHA healthcare systems for over forty years, both as a senior DoD Healthcare Administrator and a Combat-Wounded veteran, the recent scandal does not really come as a surprise; there were many warning signs over the past ten years. It was a surprise that those at the top of the organization could be unaware of the long-standing problems that so many veterans face getting access to continued care.
That General Shinseki is an extraordinary patriot is undeniable; West Point graduate from poor second-generation immigrant family, first Asian American four-star General, the first Asian American in several High-level Military and government positions, including his latest as VA Secretary. That he has served bravely is also without doubt; on the field in Vietnam he came through the 95th Combat Evacuation hospital, coincidently at the time when I had the honor to serve there as the Executive Officer, and in the political arena, the courage to speak truth to power, warning that the Rumsfeld “plan†to pacify Iraq was inadequate and would require years and over a hundred thousand troops on the ground, which cost him his job. His position was later vindicated as troop levels grew annually until they peaked at around 158,000 in 2008, following several years of failure to contain the growing insurgency and religious civil war.
There have been hundreds of hours of talking head commentaries about the scandal on all the news channels and outlets. It is surprising that while there is criticism flowing in from both sides of the aisle in Congress, some key questions concerning oversight have not been asked, including:
1)Â Â Â Â Â Were there warning signs about serious problems in the intake and continuity of care?
2)Â Â Â Â Â Who is responsible for oversight?
3)Â Â Â Â Â How can oversight be improved in the future?
1. Were there warning signs about serious problems in the intake and continuity of care?
Previous Scandal and OIG Warnings
As we watched this problem unfold, it brought to mind the widely reported 2007 Walter Reed scandal, which resulted in the Secretary of the Army’s resignation as well as the replacement of the commanding officer and several others at Walter Reed Army Medical Center. At the time, Congressional members also spoke out with indignation, crying for blood and promising to fix the system, and then went quiet.
The Office of the Inspector General (OIG) has produced 18 reports since 2005, according to this USA Today article:
“The Inspector General’s Office (OIG) said the problems it is finding are not new. It has issued 18 reports dating to 2005, documenting delays in treating veterans at some of the agency’s 150 hospitals and 820 clinics and detrimental health impact these delays have had on these patients.â€
 The VA budget shows a $121 million line item allocated to the OIG in 2015. These reports are produced as a management tool and should be used to improve healthcare access, quality and cost for veterans. They are meant to be a neutral assessment of how the organization is performing, providing an unbiased view that should probably be taken more seriously given the resources to produce them. Because the final reports come out several months or even years after the research and everyone is aware of the major findings, it is common that the hospitals answer that they have already fixed the deficiencies and they wait until the next inspection to fix the issues, if they do at all.
The VA budget shows a $121 million line item allocated to the OIG in 2015. These reports are produced as a management tool and should be used to improve healthcare access, quality and cost for veterans. They are meant to be a neutral assessment of how the organization is performing, providing an unbiased view that should probably be taken more seriously given the resources to produce them. Because the final reports come out several months or even years after the research and everyone is aware of the major findings, it is common that the hospitals answer that they have already fixed the deficiencies and they wait until the next inspection to fix the issues, if they do at all.
The White House Should Have Known
The White House also had plenty of opportunities to identify and address the brewing problems; as revealed in this hard-hitting Washington Times May 21 Report:
“According to the documents, the VA inspector general told the Obama transition team of three audits dating back to 2005 that revealed significant problems with wait times and scheduling.
One of those audits showed an instance in which the department reported 2,900 veterans waited more than a month for medical appointments. The actual figure was closer to 28,000 veterans, according to the auditors.â€
Also, it should be highlighted that Senator Back Obama sat on the US Senate Committee on Veterans Affairs, during his short tenure in the US Senate.
Internal Mechanisms Failed at Every Level
Reading through the above USA Today article, it is pretty clear that the internal mechanisms for measuring performance are broken or being manipulated for compensation reasons, and maybe they are measuring the wrong things altogether; incentives around the speed of turnaround times and volume of care delivered are quickly being replaced as the industry moves to measure quality of care with increased accountability and affordability.
Without minimizing the failure of the senior leadership to address the obvious problems (at least to those outside the organization), there were serious issues in process, systems, training and communication that all impacted the VA’s ability to deliver timely care. However, there are no credible excuses to explain the apparent lack of awareness on the part of senior officials.
As with most of these types of scandals, it boils down to ignorance or complicity, neither of which is acceptable when hundreds of billions in taxpayer dollars have been provided for the best treatment possible.
External Performance Measurement Mechanisms
Mixed Messages
Other External Evaluations include those required for accreditation and certification, the most important being the Joint Commission (TJC), which has enjoyed a longstanding congressionally mandated quasi-monopoly to accredit VHA hospitals. Whether this monopoly has been a detriment or benefit is debatable, what is not is that TJC listed the Phoenix VA Medical System first on their list of highest performers in 2010, an accolade which was quoted by the Secretary in the following Press Release:
FOR IMMEDIATE RELEASE
September 14, 2011
Twenty VA Medical Centers Make
The Joint Commission’s Top Performers List
WASHINGTON – Twenty Department of Veterans Affairs (VA) medical centers from across the Nation were recognized by The Joint Commission today as Top Performers on Key Quality Measures for 2010.
“We at VA are very pleased with the recognition from The Joint Commission. We are proud of the medical centers that made this list, proving VA’s commitment to performance measures, transparency, and accountability,†said Secretary of Veterans Affairs Eric K. Shinseki. “This achievement demonstrates our dedication to being the provider of choice for Veterans.â€
While all 152 VA medical centers are accredited by The Joint Commission, today’s list recognizes medical centers that are top performers based on The Joint Commission’s review of evidence-based care processes that are closely linked to positive patient outcomes. The 405 facilities on the list were identified for attaining and sustaining excellence in accountability measure performance for the full previous year (2010) and represent approximately 14 percent of The Joint Commission-accredited hospitals and critical access hospitals that report core measure performance data.
“VA health care has been a leader in performance measurement, electronic health records, research and clinical quality for more than a decade,†said Dr. Robert A. Petzel, VA’s under secretary for health. “I am proud of the staff and I fully expect to see more VA medical centers making this list next year.â€
The list of VA Medical Centers on the Top Performers on Key Quality Measures for 2010 includes:
- Phoenix VA Health Care System; Phoenix, Ariz.
- Nineteen Others Listed
 While the TJC awards are based on clinical outcomes, ultimately the results from thousands of assessment surveys and consulting engagements conducted during their monopoly should have uncovered the obvious, widespread failures in admissions and continuity of care. Over the last ten years, the agreement with TJC would represent the 150 hospitals and 800+ clinics each being surveyed three times. The Survey process includes at least two important inputs that should have uncovered widespread mismanagement and multiple bookkeeping: The Tracer Process and the Public Comment period. The tracer takes random patient files and follows the continuity of care at each step in the process, from ER or admission to discharge and follow up. At Phoenix it could (should) have identified patients that were seen once or requested first-time appointments, but did not have any follow up activity in their records. The process is also supposed to solicit input from the Public through public comments prior to accreditation in every facility; to suggest there was no input seems unlikely given the thousands of vets who fell through the cracks. The big picture of what is needed at VHA is a balance of Access, Quality and Cost. Benefits touted on the TJC website, include:
While the TJC awards are based on clinical outcomes, ultimately the results from thousands of assessment surveys and consulting engagements conducted during their monopoly should have uncovered the obvious, widespread failures in admissions and continuity of care. Over the last ten years, the agreement with TJC would represent the 150 hospitals and 800+ clinics each being surveyed three times. The Survey process includes at least two important inputs that should have uncovered widespread mismanagement and multiple bookkeeping: The Tracer Process and the Public Comment period. The tracer takes random patient files and follows the continuity of care at each step in the process, from ER or admission to discharge and follow up. At Phoenix it could (should) have identified patients that were seen once or requested first-time appointments, but did not have any follow up activity in their records. The process is also supposed to solicit input from the Public through public comments prior to accreditation in every facility; to suggest there was no input seems unlikely given the thousands of vets who fell through the cracks. The big picture of what is needed at VHA is a balance of Access, Quality and Cost. Benefits touted on the TJC website, include:
- Provides a framework for organizational structure and management – Accreditation involves not only preparing for a survey, but maintaining a high level of quality and compliance with the latest standards. Joint Commission accreditation provides guidance to an organization’s quality improvement efforts.
- Provides practical tools to strengthen or maintain performance excellence – The Leading Practice Library offers good practices submitted by accredited organizations. The Targeted Solutions Tool, an interactive web-based tool from the Joint Commission Center for Transforming Healthcare, allows accredited organizations to measure their organization’s performance and help them find customized solutions for challenging health care problems.
A Long History of Questionable Performance
Founded in 1951, TJC (previously JCAHO) is the largest external accreditation entity in Healthcare, enjoying a virtual monopoly in the industry for many years based on a Congressional mandate. According to their website, they currently accredit 20,500 facilities and programs. TJC also maintains a very large consulting organization, which is responsible to help clients prepare for and pass the Surveys. If it sounds like there may be a possibility of a conflict of interest, we can be comforted by a firewall that separates the consulting business from the survey business. Growing to be the largest and most powerful accrediting entity did not come without some bureaucratic lethargy over time, and by the post-911 period, Government Accountability Organization (GAO) reports detailed large percentages of accredited hospitals that had serious deficiencies based on validation exercises:
“In a sample of 500 JCAHO-accredited hospitals, state agency validation surveys conducted in fiscal years 2000 through 2002 identified 31 percent (157 hospitals) with serious deficiencies; of these, JCAHO did not identify 78 percent (123 hospitals) as having serious deficiencies. For the same validation survey sample, JCAHO also did not identify the majority (about 69 percent) of serious deficiencies found by state agencies. Importantly, the number of deficiencies found by validation surveys represents 2 percent of the 11,000 Medicare COPs surveyed by state agencies in the sample during this time period. At the same time, a single serious deficiency can limit a hospital’s capability to provide adequate care and ensure patient safety and health. Inadequacies in nursing practices or deficiencies in a hospital’s physical environment, which includes fire safety, are examples of serious deficiencies that could endanger multiple patients.†– GAO-04-850 Medicare Patient Safety in Hospitals, July 2004
2. Who is responsible for oversight?
This answer to this question is complicated. There is a relationship between Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid (CMS) and the Veterans Administration (VA). The VA Secretary reports directly to the President and there are Congressional Committees in place to provide oversight. This is on the administrative side. The short answer is that the President is responsible with input from Congress.
On the Clinical side there are myriad State and Federal regulations that must be followed relating to worker health, drugs, safety and security, organ transplantation, etc.
As detailed above, to provide input on VA performance Congress has access to a few sources to inform their oversight:
a)Â Â Â Â Â Office of the Inspector General (OIG) reports. In short, the challenge with these is they are usually published two years after the research and all of the deficiencies are claimed to be fixed based on a system of inaccurate self-reporting.
b)Â Â Â Â Â Reporting from the VA itself should be a source of performance data, but this has been shown to be flawed through omission of information or commission of fraud.
c)      Several external accreditation and certification organizations, the most important being the TJC, which enjoyed a long, congressionally-mandated monopoly that has been given to CMS. This monopoly seems to have transferred entirely over to the VA’s approximately 150 hospitals and 850 outpatient clinics, despite TJC’s documented underperformance, and CMS’ move to increase competition.
Given the huge resources and effort required to maintain accreditation across all these facilities, TJC should be able to provide the best intelligence to Congress on what is actually going on inside every hospital in the organization; the primary input for Congressional oversight. This would be a foregone conclusion if they had found the fraud and broken processes at the Phoenix VA Medical Center, rather than declaring them one of the Top 20 in the country.
3. How Can Oversight Be Improved in the Future?
Looking back on the three main sources of input for Congress to use for its’ oversight responsibilities, we would recommend the following as a minimum approach to improve the system:
- Take advantage of the existing OIG reports
- Use them in a defined process that actively looks at the recommendations
- Increase the number of validations using small samples to identify problems sooner and focus on high impact areas, with quick turnaround.
- Shake up the organization with Red Team Inspections; unannounced visits the day after new accreditation has been awarded – Do not rely on self-reporting
- Listen to the Customer – contact 100 new patient files and have them rate the satisfaction level of getting access, follow up care and discharge instructions.
- Reform the Management of the VHA for Increased Accountability
- If the leader is military, they should have a deep background in providing healthcare, it is not a position that “checks the boxes†to get things done from top down, it requires an understanding of service delivery with leadership that can convince, not coerce people into doing the right thing.
- Leadership should review the processes for intake and follow up appointments and make sure it is balanced against available resources. If it is not reasonably possible to meet a target of 14 days for an appointment, then the target should change or the process should be fixed.
- Leadership should shake the organization out of its’ complacency, anyone with fingerprints on the double filing system and their direct supervisor should be fired. Civil Service is not a meal ticket for life; the private sector has been decimated by market forces and there is no room for a nine-to-five attitude for those who want to keep their jobs and substantial benefits that have disappeared in the private sector. An example: after experiencing serious issues getting specialty care through a very unresponsive Nursing help line, I escalated to the Director of a VA Medical Center and sat with him, explaining in detail. In the conversation I suggested we call the help line or listen to the quality control recordings, stunned at the answer that the union would not allow recording of calls or calling with the purpose of doing an ad hoc assessment. How can you manage quality of a call service without listening to the calls and holding people accountable for rude behavior or lack of follow up? The only way to manage a process is to measure it and improve based on valid data. Unfortunately, the vast majority of vets will not escalate the issues because they do not understand the bureaucracy and are afraid of angering their primary provider of care. In real life, if they don’t escalate a follow-up appointment for a GI exam, they could end up with Stage 4 colon cancer and require a million dollars of care, and still not survive. The majority of staffers are individually very courteous and dedicated, but there is an overall culture that allows things to slip through the cracks that needs to be addressed. And fraud should have serious consequences.
- These issues make VA a less desirable place to work for physicians and nurses, which in turn can impact the quality of care and the efforts to recruit talent into the system. Improvement of patient access, patient satisfaction and internal accountability will also improve job satisfaction and recruiting efforts.
- It will be important to have a respected, hands-on operator in the leadership role, one who understands the limitations of the bureaucracy, how fraud and waste impact the quality of services, and the needs of patients when receiving quality healthcare. This should be a non-partisan issue. We feel that retiring Senator Tom Coburn of Oklahoma would be a good choice for the administration to tap for the open position, given the senator’s background, training and willingness to cross the aisle for issues of importance.
- Introduce Better Quality and Accountability in External Evaluation Mechanisms
- The VA’s exclusive external evaluation provider, TJC, missed the failures at Phoenix, actually awarding it a Top Performer accolade in 2010 and during the 2007 Walter Reed scandal mentioned above (that brought down the Secretary of the Army), Walter Reed Medical Center had been accredited with flying colors. While we understand that it is easier for VA to push everything related to accreditation (hospitals, labs, medical programs, pharmacy, etc.) to a single provider over a long period, a result that is typical in any business is that lack of competition and conflicts of interests result in lower quality deliverables to the end customer. Currently, VHA accreditation awards are written in a way that makes it impossible to be considered for those who do not offer every single requirement that is listed in the needs document. Communicating with VA on these awards is like speaking into a black hole; nothing ever comes out. Our company does not offer accreditation services but we do offer SME consulting on a subset of requirements in the areas of All Hazards Readiness. All Hazards Readiness has largely been underserved by the TJC standards over the years. Opening up this accreditation monopoly to another firm or team of firms to begin leveling the playing field, might be a little harder to manage for VA’s compliance team, but we believe the benefits of increased competition, higher quality results and better transparency would be apparent.
- The internal process of how the Accreditation Awards are validated should be documented and built into a process that ensures that adequate work is being done in this massive government contract, For example:
i.     Taking the Walter Reed Accreditation prior to the 2007 scandal and finding out how the substandard conditions at the facility were missed and how the Hospital received high marks in the accreditation.
ii.     Looking at the latest Accreditation award for the Phoenix VA Medical Center and finding out how many tracers were performed and how the double set of books was missed.
iii.     Understand using these two examples how the organization could be missing “the forest for the trees†in the current quality control and making appropriate changes internally at VA, and within the Accreditation Process to prevent this from happening in the future.
iv.     Fully half of the Iraq and Afghanistan vets are coming home and claiming disabilities, we are just seeing the front-end of a lifetime of care for these vets, through the VA.
v.     This is a sixty year commitment that puts even more pressure on an already stressed system. We believe the unintended consequences of moving towards a voucher system as a long term solution might outweigh the benefits in the already-stressed healthcare delivery system.




0 Comments