The recent CNN Opinion piece “Bringing medical misdeeds into the light†ruffled the feathers of the 6,000 members of the American Society of Healthcare Risk Management (ASHRM). The article came to the author’s attention at a time when he had drafted comments on a review of the ASHRM/American Health Lawyers Association (AHLA) second edition of ENTERPRISE RISK MANAGEMENT HANDBOOK for HEALTHCARE ENTITIES, 2013. I have been an active member in ASHRM since 2005. It has been our practice at the Center for HealthCare Emergency Readiness (CHCER) to keep close relationships with professional organizations which play a pivotal role in healthcare all-hazards preparedness. Comments on the handbook will be covered in detail as an official reply to the request for comments and published at www.chcer.org. and in later posts.
It would be instructive to take the time and review the public comments on the article. The vast majority of comments were directed toward caregivers in general, missing the point that the clinicians are being marginalized in the risk management process. The vast majority of ASHRM professional hospital risk managers are Nurses. The dominant focus is in the clinical domain and they play an indispensable role in all aspect of clinical patient safety.
Their professional role is among the most challenging in the healthcare industry. Those who are Nurses must be full-time Clinical Nurses, part-time Hospital Administrators, Lawyers, Insurance experts, Press Agents, Public Safety Officers etc. In the last two decades of my “boots on the ground†hospital career, I find these individuals in the role of clinical risk managers to be among the brightest most dedicated members of the organization.
Over the last thirty years the role of the Risk Manager (and particularly Nurses in this capacity) has moved from one that was focused on economic impact from liability to an overarching concern for any risk that could damage the institution, its reputation, financial liability and legal vulnerability. Simultaneously, as the risk profile has changed, the tendency to move decisions away from clinicians and toward lawyers and non-clinical risk managers has increased, squeezing clinicians (especially nurses) in the process; Clinicians still have the public facing profile while having less and less influence on the final disposition.
“First Do No Harmâ€
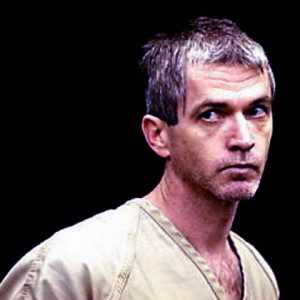
The above-mentioned CNN article refers to the Cullin case, which involved a 16 year criminal nursing career which resulted in 40 known and perhaps 100 murders within several hospitals in New Jersey and Pennsylvania. A video documentary of his killing spree can be seen here. Shocking as this is, it is just another statistic in the recent history of serial killers in the guise of professional caregivers, According to the Journal of Healthcare Protection Management, between 1970 and 2006, 90 criminal prosecutions of healthcare providers uncovered that 54 caregivers were responsible for 2013 murders in hospitals and nursing homes. Of the 54, 45 were convicted of serial murder, 4 for attempted murder and 5 pleaded guilty to lesser charges.
In light of this revelation, several points come to mind:
1)Â Â Â Â Â As recently as 2008, up to 1/3 of California caregivers had not undergone a criminal back ground check at time of employment, including 75% of psychiatric technicians, 50% of all family therapists, social workers and dentists and 12% of all physicians (Orstein and Webber, LA Times 12/2008)
2)     The 20 year National DHHS database of caregiver offenders (Nurses, Pharmacists, Psychologists, etc., had turned up missing at the time of our book “Unready†in 2010
3)      A recent Survey published by Healthcare Finance News “Barriers to Patient Safety Still Existâ€, reported that although 96% of the C-Suite and Risk Managers say their hospital has a culture of patient safety, 1/3 (33% C-Suite & 37% Risk Managers) acknowledged that their hospital needs to undergo major changes to maintain that culture.
The approach to Risk Management which quietly shuffles dangerous caregivers in one hospital to vulnerable patients in another is a practice which is ethically, morally and legally repugnant. As long as there are positive consequences to this behavior, it will continue unabated. Â The big questions here are who can make the change and when will they begin?






0 Comments