 We congratulate the Tuscon AZ response team from first responders to the AZ Medical Center ER, to all levels of clinical treatment. The limited scope of the tragic shooting incident allowed for the treatment of all victims in a timely manner. Unlike larger mass casualty events, all victims were properly treated and evacuated to the area Medical Center. Resources were available to care for all, the near-dead, seriously wounded, lightly wounded and walking wounded. without having to resort to a “ mass casualties triage†where painful decisions about who could be saved and who would be left behind. Even so, the Medical facility was stressed but did not have to reduce their traditional standard of care.
We congratulate the Tuscon AZ response team from first responders to the AZ Medical Center ER, to all levels of clinical treatment. The limited scope of the tragic shooting incident allowed for the treatment of all victims in a timely manner. Unlike larger mass casualty events, all victims were properly treated and evacuated to the area Medical Center. Resources were available to care for all, the near-dead, seriously wounded, lightly wounded and walking wounded. without having to resort to a “ mass casualties triage†where painful decisions about who could be saved and who would be left behind. Even so, the Medical facility was stressed but did not have to reduce their traditional standard of care.
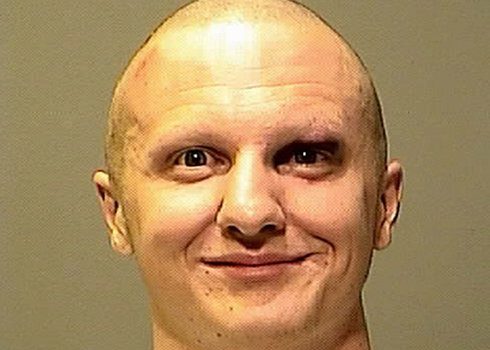
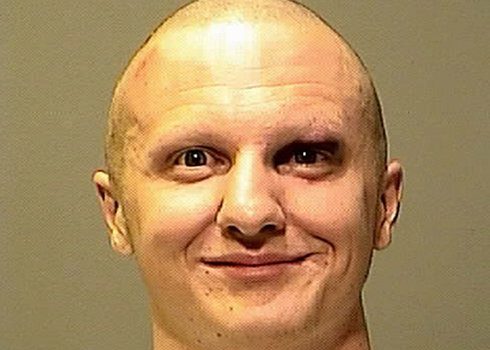
We have had a week of expert? testimony about: How could this tragic event have been prevented; What if someone had detected and reported the bizarre behavior to proper mental health authorities in a timely manner?; Were those resources available? ; What were the barriers to law enforcement community to identify s shooter as a community risk?
It appears that a vigilant Wall-Mart clerk refused to sell the shooter ammunition and another sales clerk in the area had little concern about such a sale. Why did a gun store salesperson feel that he could not legally refuse to sell the gun and super magazine? If extant laws posed these barriers to timely identification and weapons purchases then what does that mean for the trusting public?
If authorities are not willing to change the laws then the only alternative is to be prepared to respond to these random events. The Mental Health community tells us that there are upward to 4 million seriously ill individuals in the population who could act out in very dangerous ways. There are very few communities with the same level of response capabilities as were available in Tuscon.
Contrast that to a Mumbai-style attack with hundreds of casualties with a range of wounds, some fatal, some near-fatal, walking wounded and worried well. In Mumbai the receiving hospitals were under direct attack with running gun and grenade battles adding to the casualties and denying timely organized care for all casualties.
Back to External Evaluation Mechanism for Emergency Management after the 2008 nine month hiatus of not scoring for essential elements to determine all-hazards response for hospitals (TJC). (see previous article on “To the Rear Marchâ€)
The Center for Medicare and Medicaid Services (CMS) assesses the effectiveness of their contracted hospital external evaluators through periodic “Validation Surveys†performed by State Survey Agencies. CMS has limited oversight authority over JCAHO’s hospital accreditation program because of the program’s unique legal status effectively prevents CMS from taking actions that it has authority to take with other accrediting bodies.
“Validation Surveys†performed by State Survey Agencies. CMS has limited oversight authority over JCAHO’s hospital accreditation program because of the program’s unique legal status effectively prevents CMS from taking actions that it has authority to take with other accrediting bodies.
These “Validation Surveys†(VD) have been significantly curtailed this last decade, however, a two year sample of 500 JCAHO accredited hospitals identified alarming deficiencies missed by the JCAHO surveys (GAO-04-850). Eighty-seven (87) of the One hundred sixty seven (167) serious deficiencies were related to hospital’s physical environment. Weakness in assessments of these standard elements were evident in the Katrina and Ike responses and continue to surface in the failure to enforcement of the E.C. standards in 2008.
Emergency Management (EM) enjoyed a higher profile in the The 2009 TJC standards. A stand alone Chapter with its own set of of Elements of Performance EPs). TJC periodic reports which surface challenging areas of standards compliance did not identify all-hazards preparedness (Emergency Management) as troublesome areas. They did surface concern for the safety and security of healthcare caregivers. Personal assaults on women caregivers have more than tripled in recent years. Hospital shootings have been on the rise. Physical violence in the workplace has pushed the sector into one of the nation’s most dangerous work sites.
The threats come from many quarters, lack of access control, weak employment screening, increased outsourcing, downsizing of security force etc.
We have been spending a lot of time on quality and reliability of TJC safety and security external evaluation of hospitals There are others and we would hasten to  add that none of the extant external evaluation mechanisms for healthcare emergency management have yet to develop assessment schemes which come close to approximating an acceptable level of readiness envisioned by the National Response Framework (NRF).
add that none of the extant external evaluation mechanisms for healthcare emergency management have yet to develop assessment schemes which come close to approximating an acceptable level of readiness envisioned by the National Response Framework (NRF).
Personal observations and scattered reports from trade organizations question the selective reporting which leads one to believe that the all-hazards emergency management gap has been addressed. We see evidence of a wholesale trend to de-emphasize the efforts to hold hospitals accountable for E.M. compliance. The May 19, 2010 Joint Commission Online announces the deletion of the requirement to document “Measures of Success†associated with Elements of Performance, among them over 20 Environment of Care Standards.
The formal removal of the “Emergency Management Tracer†which followed the very
successful model “Clinical Care Tracer†to evaluated quality of care, is indeed unfortunate and does not bode well for an in-depth evaluation of all-hazards readiness.
The January, 2010 report funded by the DHHS provides us with a current overview of the Nation’s Hospital and Healthcare readiness to deal with known hazardous threats.
The Next Challenge in Healthcare Preparedness: Catastrophic Health Events, Changing the name “ Weapons of Mass Destruction (WMD) or All-hazards Readiness †to “Catastrophic Health Events†does not erase twenty years of Healthcare Industry Apathy, Denial and Cognitive Dissonance.(old wine in new bottles).
The Administration’s characterization of the “National Health Security Strategy of theUnited States of America†as the first call to the healthcare industry to prepare for all-hazards readiness is inexplicable.
Along the continuum of human errors are legitimate mistakes and a range of “sins of Commission and sins of Omission†From where I sit, “sins of Ommission “ are much more harmful to the public good, and take less personal courage. JB
This article was adapted from excerpts from Blair’s book, Unready: To Err is Human: The Other Neglected Side of Hospital Safety and Security, which was published in June. He is also a career-retired army colonel with 28 years of active service. Among his private sector experiences, he served as VP of Hospital Corporation of America, Middle East Limited and as an independent consultant to Joint Commission International.





0 Comments